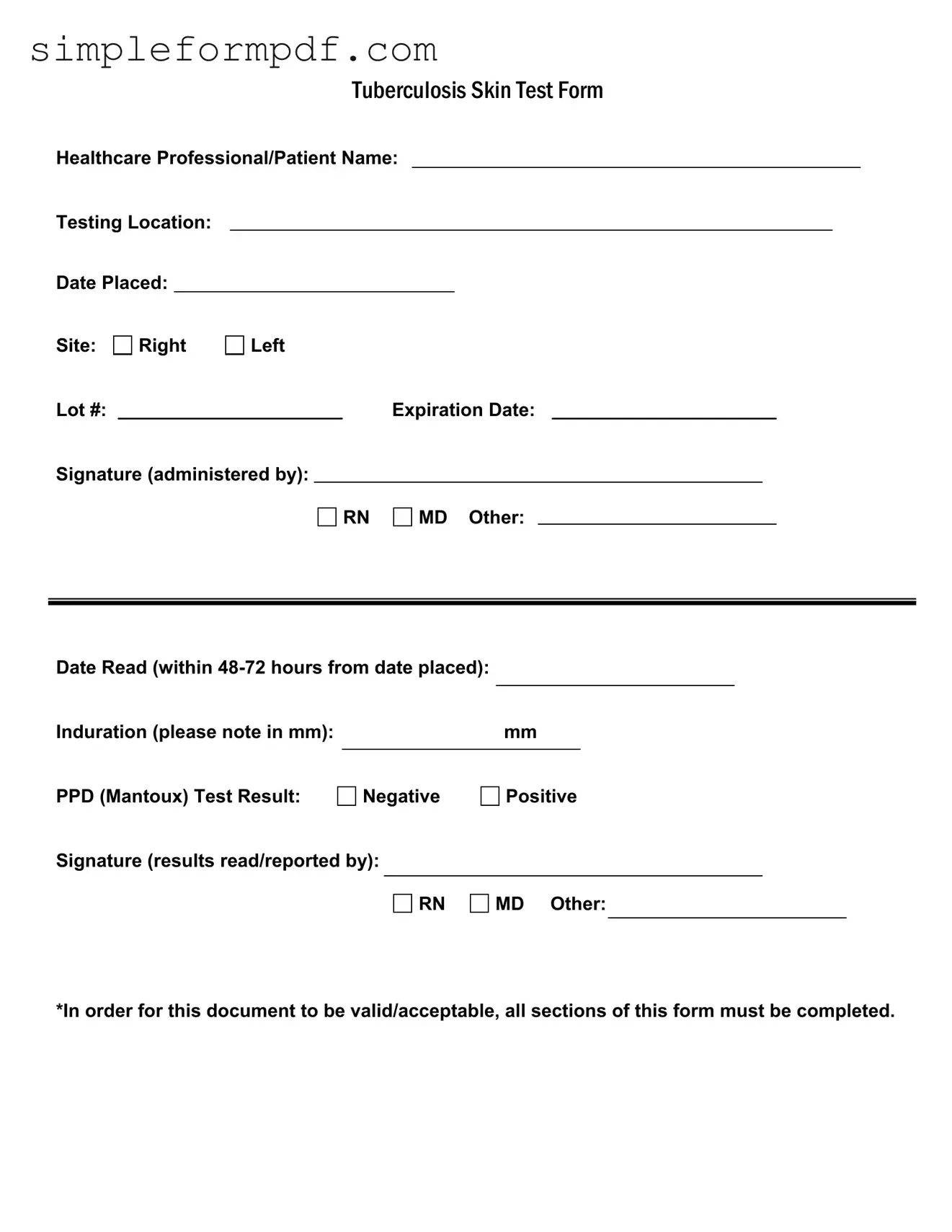
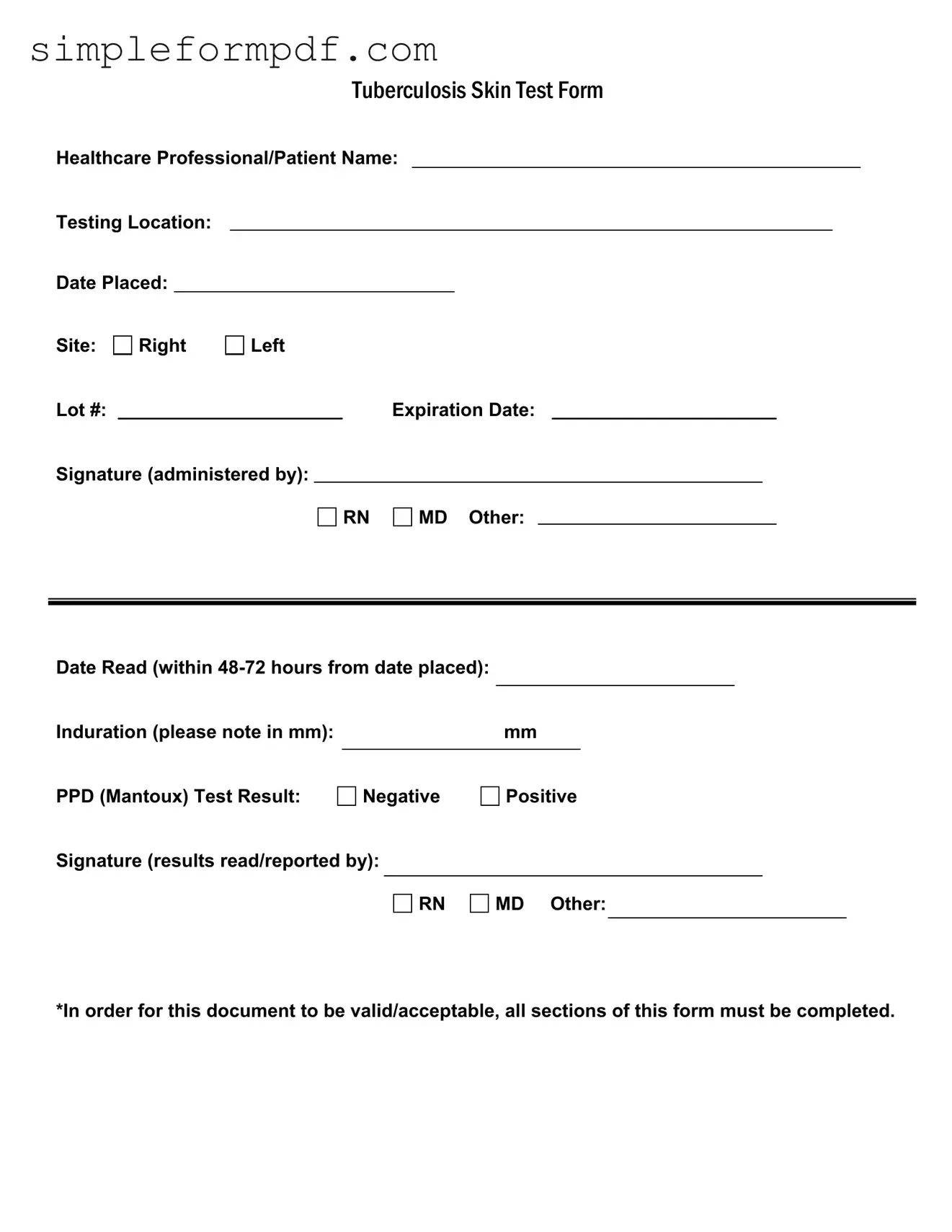
Tb Test PDF Form
The Tuberculosis Skin Test Form is a vital document used to record the details of a tuberculosis screening. It includes essential information such as the healthcare professional's name, testing location, and results of the test. Completing this form accurately is crucial for ensuring proper documentation and follow-up care.
If you need to fill out the form, please click the button below.
Launch Editor
Tb Test PDF Form
Launch Editor
Need instant form completion?
Finish Tb Test online in just a few minutes.
Launch Editor
or
Download PDF