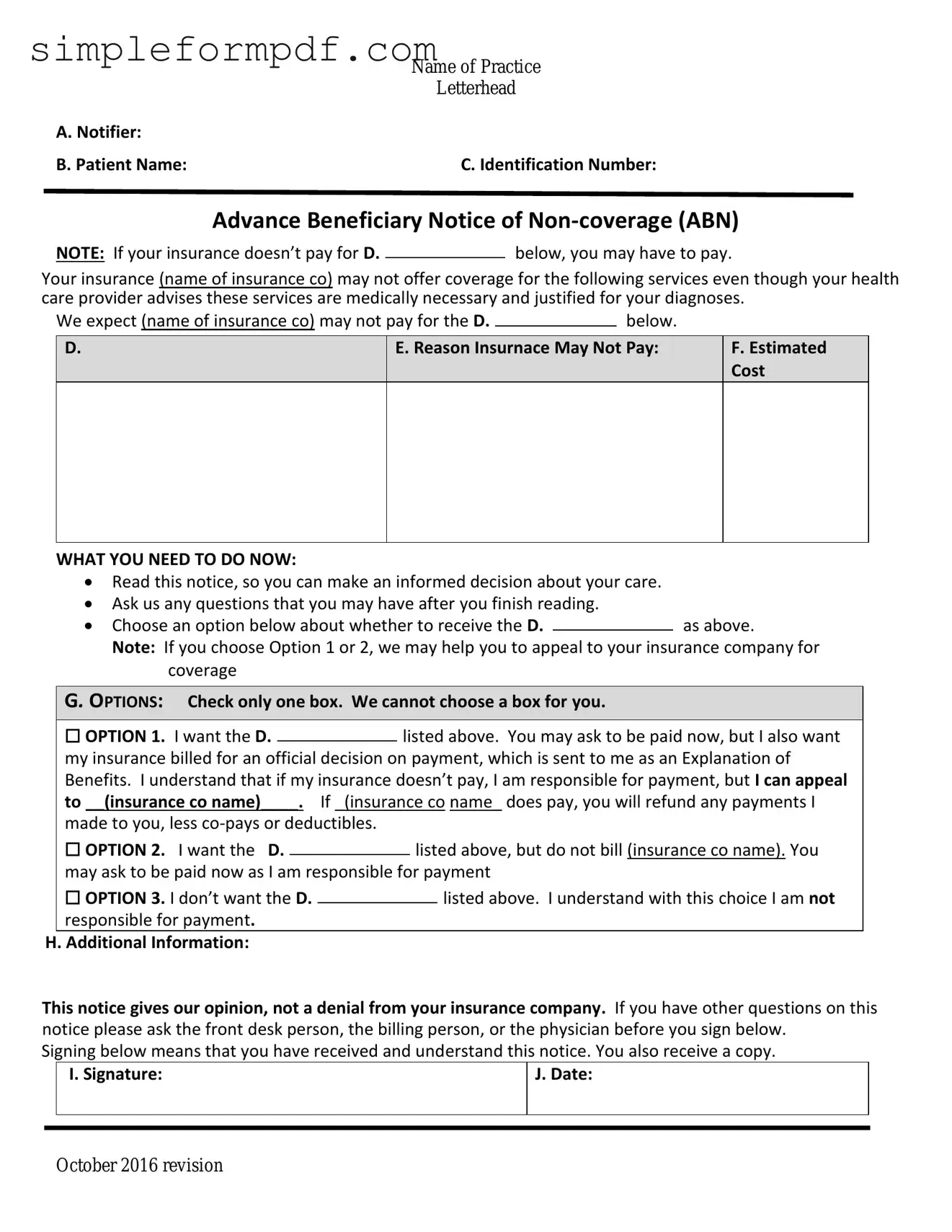
Advance Beneficiary Notice of Non-coverage PDF Form
The Advance Beneficiary Notice of Non-coverage (ABN) is a crucial document that informs Medicare beneficiaries when a service or item may not be covered by Medicare. This notice allows patients to make informed decisions about their healthcare and potential out-of-pocket costs. Understanding this form is essential for navigating Medicare effectively, so take action now by filling out the form below.
Launch Editor
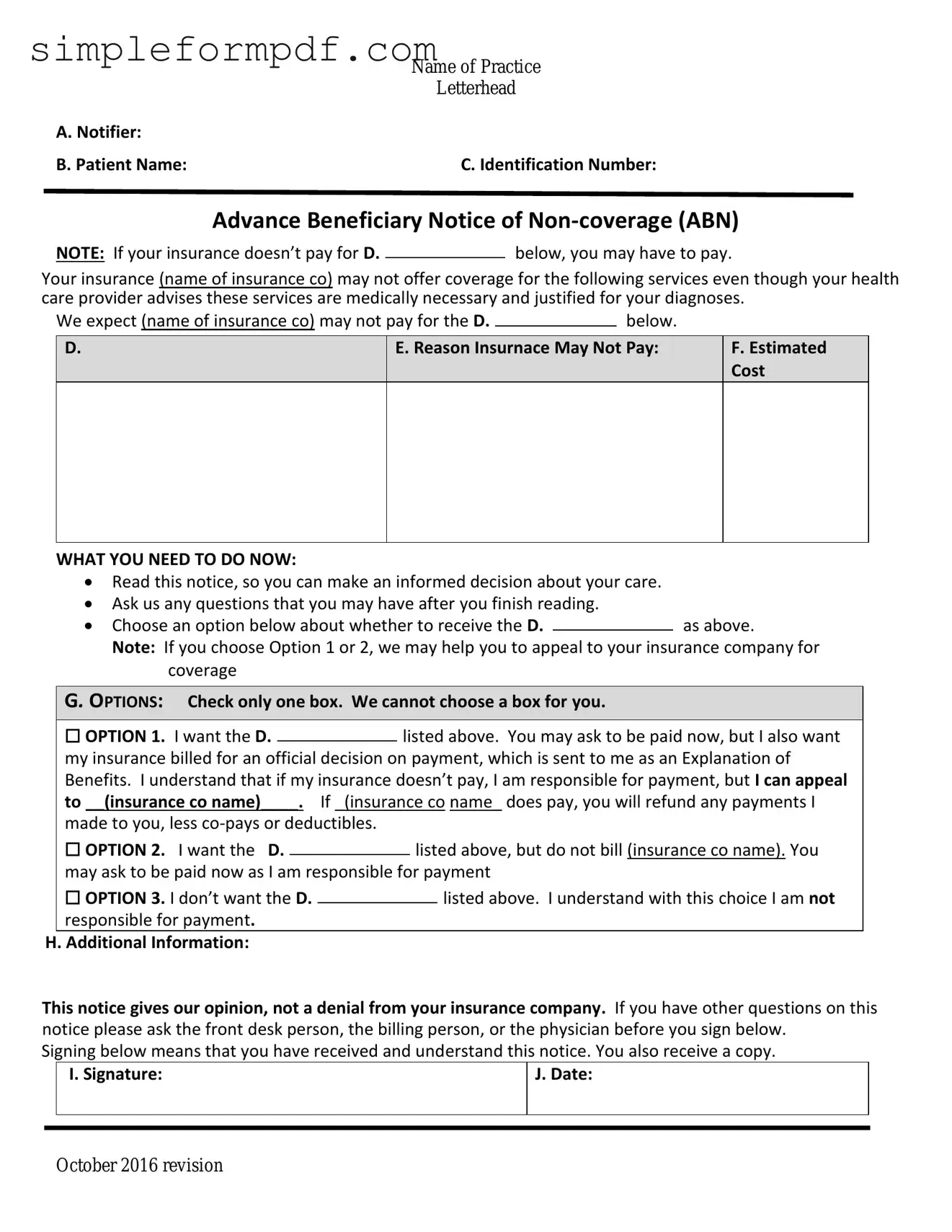
Advance Beneficiary Notice of Non-coverage PDF Form
Launch Editor
Need instant form completion?
Finish Advance Beneficiary Notice of Non-coverage online in just a few minutes.
Launch Editor
or
Download PDF